Nestled in the heart of Kwale County, in Msambweni Sub-county, lies Mwamanga village—a quiet and lush settlement that forms part of the Bongwe community unit, home to 4,320 people.
The journey into Mwamanga is marked by serene silence and the gentle rustle of tall green trees that tower over the area. Almost every homestead boasts mango trees, their branches heavy with ripe fruit. Fallen mangoes carpet the ground.
Boda bodas serve as the main mode of transport. Schools and health facilities are few and far between, and signs of public services are scarce.
Deep in this rural quietude lies Mwamanga Junior School—a beacon of learning and promise. It stands on a large parcel of land, its grounds buzzing with the energy of children. Their faces light up with curiosity as visitors walk through the gates and into their classrooms.
Inside one classroom, an unusual setup catches the eye. Seated at a desk near the front of the room is Keziah Gitonga, a medical laboratory officer. Her workspace is carefully arranged: a red polythene covers the table on which various tools—scissors, surgical spirit, and rapid diagnostic kits—are neatly laid out.
A blood test is in progress. A team of health workers are part of an effort to trace the footprints of a disease that has ravaged this region for decades—Lymphatic filariasis commonly known as elephantiasis. It is a disease caused by parasitic worms transmitted through mosquito bites.
Inside the classroom, a group of six and seven-year-old children wait patiently as clinicians prick their fingers for blood samples. It’s a simple test, taking just ten minutes to yield results, but it carries profound significance.
These children were born during a period of aggressive mass drug administration (MDA) campaigns. If any of them test positive for filarial worms, it could indicate that transmission is still occurring—suggesting that some community members may have slipped through the cracks of previous interventions.
- Africa's health future in focus at AHAIC 2025 amid US aid freeze
- Time to embrace the healing power of music, it can also motivate you
- Early detection: Lucy's cervical cancer journey and key lessons for you
- Concern as mystery disease kills over 50 people in DRC
Keep Reading
“This age group is critical,” explains Keziah Gitonga, “They were born when the area was receiving annual MDA treatments for seven consecutive years. If they test negative, it confirms there has been no recent transmission.”
Lymphatic Filariasis is a neglected tropical disease (NTD) caused by parasitic worms transmitted by mosquitos. Over time, the worms damage the lymphatic system, leading to severe swelling in limbs, breasts, or genitals—a condition commonly referred to as elephantiasis. The disfigurement is not only painful but also emotionally and socially devastating, often leading to stigma and isolation.
Globally, over 120 million people in 72 countries are affected, mainly in impoverished regions of Africa, Asia, the Pacific Islands, the Caribbean, and South America.
The World Health Organisation (WHO) launched the Global Programme to Eliminate Lymphatic Filariasis in 2000, delivering more than 9.7 billion treatments worldwide in 71 countries. As a result, 33 countries have reduced infection prevalence to levels where transmission is no longer sustainable, with 21 having eliminated LF as a public health problem.
In Kenya, LF is endemic in all six coastal counties, with Kwale County bearing the highest burden. A recent community mapping identified over 2,000 individuals suffering from lymphedema due to LF.
Kenya is endemic to 19 of the 20 NTDs recognised by WHO, having been certified free of guinea worm disease in 2018. The country is developing a new plan to control and eliminate NTDs, with LF and blinding trachoma earmarked for elimination as public health threats by 2027.
In Mwamanga and other parts of Kwale County, many have witnessed the toll of the disease. Traditionally attributed to witchcraft, elephantiasis has been a source of shame for many families. But thanks to continuous community education efforts, perceptions are changing.
“Now people understand it is a disease caused by mosquitoes, not a curse,” says Keziah. “That shift in knowledge is helping reduce stigma.”
In the past decade, the Ministry of Health has implemented seven rounds of MDA in Kwale, distributing anti-filarial medications annually. The treatment, which includes drugs such as ivermectin and albendazole, is designed to clear the parasitic worms from the bloodstream and preventing new infections.
During the first phase, known as Task 1, MDA was administered across the region, targeting the entire eligible population. “We saw a lot of progress then,” Keziah recalls. “People responded well, and symptoms started to decline.”
But that wasn’t the end. Following Task 1, health officials launched Task 2, a surveillance phase to ensure no new infections were occurring. “This is why we’re testing the six to seven-year-olds,” Keziah says. “If they’re clear, it confirms that the drugs worked and there’s no active transmission. If we find any positives, it means there are still small pockets of the disease.”
If all goes well, Task 3 will begin in two years, with the ultimate goal of eliminating the disease from Kwale County by 2027. “We are hopeful,” Keziah says. “We’ve come a long way.”
The procedure is meticulous but straightforward. Children in grades one and two are selected, with informed consent obtained from their parents. “We explain why we’re only testing this age group,” says Keziah. “They represent a generation born and raised during the treatment period.”
A small drop of blood is taken from each child and placed onto a rapid diagnostic test (RDT) kit, which detects antigens produced by the parasites. “If it shows one line, it’s negative. Two lines mean a positive case,” Keziah explains.
For every positive case, a more detailed follow-up is conducted. Parents are informed, the household is visited—usually late at night when parasite levels in the blood are highest—and additional samples are collected. These are sent to a laboratory where they are examined under a microscope for microfilariae, the larval form of the worms.
“If we confirm a case, we don’t do mass treatment again. Instead, we administer targeted treatment to the household or village,” Keziah says.
But humans aren’t the only focus. The team also monitors mosquitos through a process known as molecular xenomonitoring. “We collect mosquitos from selected areas and analyse them using PCR tests to check if they carry the parasite,” Keziah explains.
This dual approach—testing both people and mosquitoes—provides a fuller picture of the transmission cycle. “Sometimes, even if people test negative, mosquitoes might still be carrying the parasite,” she adds.
Community health promoters are at the frontline of this campaign. The CHPs and Community Health Assistants (CHAs) form the backbone of a nationwide MDA campaign targeting NTDs.
At the heart of this campaign is Aisha Omar-Jungo, Mwanaisha Mwangwete and Fatuma Mohammed, a passionate Community Health Assistant who also doubles up as a Community Drug Assistant. Fatuma not only supervises the distribution of essential medication in Mwamanga but also trains CHPs on how to administer the drugs, record household data, and navigate community resistance.
“Our work starts with training,” Fatuma explains. “Once I’m trained by the sub county health team, I pass that knowledge to my CHPs, teaching them how to administer Praziquantel 600mg and Vermox Chewable 500mg, how to calculate dosages using height, and how to record the correct data for each person treated.”
Each CHP is tasked with covering approximately 100 households over a five-day period during the MDA campaign. Armed with registers, measuring tools, and often with no transportation, they walk door to door to ensure no one is left behind. In Mwamanga village alone, there are about 672 people, and within the wider Bongwe community unit, the population stands at 4,320.
The CHPs begin by introducing themselves at each household, asking for permission to explain the importance of the medication. They then proceed to measure each eligible individual’s height using a standard WHO height-dose pole to determine the number of Praziquantel tablets to give. For example, a child who is 54 inches tall receives two and a half tablets. The dose of Vermox is a standard 500mg chewable tablet.
“We don’t test before administering,” says Fatuma. “The drugs act both as preventive and curative. This is a public health intervention aimed at controlling the spread across the entire population.”
Although the campaign aims for universal coverage, certain groups are excluded from treatment for safety reasons. Pregnant women, individuals under one year, those very sick or bedridden, and people on long-term medications—especially those with immunocompromising conditions like diabetes—are not administered the drugs due to potential contraindications.
“We are cautious,” explains Fatuma. “We refer those excluded to health facilities for further evaluation and appropriate care.”
Despite the thorough training and professionalism of CHPs, some community members resist the medication due to fear or misinformation. In such cases, CHPs report the individuals to chiefs, assistant chiefs, and village elders, who are trained to step in and help educate the reluctant households.
“Rejection is rare because we do a lot of community sensitisation before the campaign,” says Hildah Mahenzo, the Msambweni Sub County NTD Coordinator. “We involve local administrators and community influencers in behavior change communication, which is vital for acceptance.”
This behavioural approach is part of the national Social and Behaviour Change Communication (SBCC) and Policy, Communication, and Coordination (PCC) frameworks—strategies designed to drive public health messages and influence attitudes around drug safety and disease prevention.
While local CHPs implement the program on the ground, the national health team provides technical support, policy direction, and training. They also handle drug procurement, health promotion, and monitoring and supervision across counties.
“After we train the county teams,” says Mahenzo “they become trainers for their sub county teams, who then train CHPs. It’s a cascade model that ensures consistency and accountability.”
Kwale County is also one of the beneficiaries of a pilot paediatric formulation project, aimed at reaching younger children previously excluded from MDA due to age or dosage limitations. This project, known as the ADOPT study, is testing child-friendly formulations of Praziquantel to close that gap in treatment.
To enhance efficiency and data accuracy, Kwale’s health team is adopting the Electronic Community Health Information System (eCHIS). CHPs use phones and tablets to input data in real-time, replacing the cumbersome paper registers that delayed reporting and risked data loss.
“With eCHIS, we can see who took the drug, where, and when—all in real-time,” explains Fatuma. “It helps with follow-up and planning future rounds of treatment.”
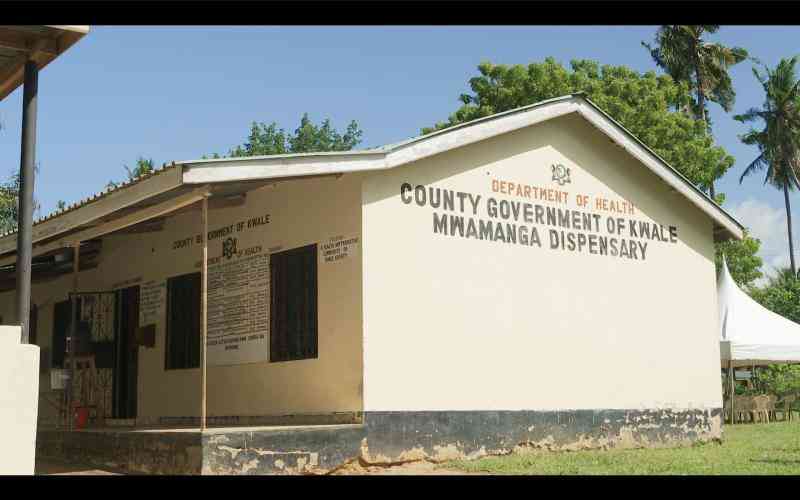
Mwamanga Dispensary stands out as a vital outpost in the fight against lymphatic filariasis. Nurse-in-charge, Salama Zani, has become a key figure in leading efforts to manage this condition, particularly among the growing number of lymphoedema and hydrocele patients. “This facility records the highest number of lymphoedema cases in the county,” says Salama. “That’s why we became the coordination unit for patient mapping, support, and care.”
With a population of around 6,000 people, Mwamanga Dispensary has established a proactive approach to support those suffering from the disease. Two months ago, the dispensary partnered with public health workers and CHPs to map affected individuals, resulting in the formation of the Tujikaze Support Group—a group now offering hope, training, and dignity to those battling the condition.
Lymphatic filariasis is incurable but its symptoms can be managed with consistent hygiene, medication, and emotional support. Hydrocele, a related condition often affecting men, involves swelling in the scrotum and carries immense stigma.
“Hydrocele patients often suffer in silence,” Salama adds. “They are referred to Msambweni Sub-county referral Hospital, the regional referral centre, for surgical intervention. While we don’t perform surgeries here, we provide counselling, link patients to hospitals, and follow up with home-based care.”
Salama notes that Msambweni leads in hydrocele cases, likely due to its proximity to endemic mosquito breeding areas and the historical neglect of the disease. She says stigma and misinformation often prevent patients from seeking care, especially men with hydrocele.
The Tujikaze Support Group comprises of 20 members, all trained in basic home-based care. Led by Bakari Hamisi, a patient-turned-advocate, the group meets bi-weekly at the dispensary to share their experiences, offer emotional support, and track progress.
“I was chosen as the chairperson of the group. At first, I had given up. I thought I was the only one,” says Bakari. “CHPs linked us to the facility and trained us. We’ve now met at least six times since the group started.”
Through the support group, patients learn essential hygiene techniques—regular washing, elevation of swollen limbs, and use of painkillers—to manage the condition. However, challenges remain, particularly the inconsistent supply of medication.
Ramadhan Mohammed, 26, has lived with lymphoedema since he was 16. “It started slowly, then the swelling became painful,” he recalls. He now lives a limited life, unable to walk comfortably or engage in consistent work.
“Sometimes at night, the pain wakes me up. When I raise the leg, it helps. But when it’s down, the pain is unbearable,” he explains.
Ramadhan also faces social stigma. “I don’t have a wife. Women avoid me because I’m sick,” he says.
Lymphatic filariasis is endemic in six counties in the coastal region, namely Kilifi, Kwale, Lamu, Mombasa, Taita Taveta, and Tana River. Approximately 3.9 million people in the region are at risk for LF.
Witchcraft
According to Salama, healthcare workers across these regions have been retrained using WHO protocols to deliver routine hydrocele surgeries and manage lymphoedema through integrated care.
Despite these efforts, budget constraints, medication shortages, and lingering community stigma continue to hinder progress. Mwanasiti Bwirira, a Community Health Assistant, stresses the need for ongoing community education.
“Acceptance is still a challenge. Many believe the disease is a curse or hereditary. We need more sensitisation to change attitudes,” she says.
Michael Ofire, NTD Programme Manager for AMREF Health Africa says stigma and poverty are intertwined obstacles. “Many believe the disease is caused by witchcraft or drinking local brew. Because of this misinformation, patients are socially excluded,” he says.
Ofire adds that although Kenya has made commendable progress—from over four million people needing preventive medication to just over 12,000—the burden of those already suffering is still severe. In Kwale alone, more than 2,000 individuals have chronic lymphoedema. “We’ve trained health workers and physiotherapists, and we’re working with county governments and the Ministry of Health to embed long-term care.”
While Msambweni and other counties have trained surgeons to perform hydrocele surgeries, budget constraints is a major hurdle. “The government only pays salaries for health workers. Donor fatigue, external debt, and recent USAID funding cuts are affecting the sustainability of our programs,” Ofire says.
He urges county and national governments to treat elephantiasis as a priority. “Eliminating lymphatic filariasis by 2027 is within reach, but only if we close the funding gaps and integrate economic empowerment into health programs,” he says.
The END Fund, a philanthropic initiative dedicated to ending NTDs, has partnered with the Ministry of Health and county governments to eliminate lymphatic filariasis by 2027.
Through this collaboration, the END Fund supports mass drug administration, surgical interventions, and community education programs aimed at reducing the disease’s prevalence and associated stigma.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.